Are crossword puzzles becoming difficult?
Can you distinguish the taste of pinot noir versus a rosé? Would you rather listen to jazz or hard rock? Do you prefer to run or lift weights for exercise? Do you like dogs or cats? Do you want to grow flowers or vegetables? To answer any of these questions, you need to use your semantic memory.
Your semantic memory is your store of factual knowledge of the world and the meaning of words. It’s how you know that a pen is for writing and a sunflower is yellow. It’s both the source of your vocabulary and how you know what something is, even if you don’t know, the name of it — like difficulty getting out of bed in the morning is called Dysania. Illegible handwriting, like yours truly, is called griffonage. Kummerspeck is the excess weight you gain from emotional eating. No sweat, I didn’t know these either!
USE EPISODIC MEMORY TO INCREASE YOUR SEMANTIC MEMORY.
Episodic memories are what most people think of as memory. They include information about recent or past events and experiences, such as where you parked your car this morning or the dinner you had with a friend last month. You need to use your episodic memory to learn new information, to form new semantic memory. For a week, month, or year, you might remember where you were and what you were doing when you learned a new fact. Over time, however, you will forget the context and recognize the fact. Once only the fact remains, it is part of your semantic memory.
YOUR BRAIN’S DICTIONARY-THE LEFT TEMPORAL LOBE.
Research has shown that semantic memory is stored in the left temporal lobe. Several landmark papers have examined where semantic memory is stored in the brain. In 1996, two related studies were published in an article in Nature. For the first, the researchers enrolled over 100 patients who suffered from stroke or other brain lesions in their left temporal lobe. (Put your finger on your left temple, just behind your eye — that’s where the left temporal lobe is located.) They asked these patients to name famous people, animals, and tools that were human-made objects. They found that the location of brain lesions affected recall. Patients with the most anterior lesions (close to their eyes) had the most significant difficulty naming persons. Patients with the most posterior lesions (toward the back of the head) had the greatest problem naming tools. And those with lesions in between these areas had the most difficulty naming animals.
In the second study, the researchers had healthy adults name famous people, animals, and tools while undergoing a positron emission tomography (PET) scan that showed brain activity. As expected, naming people yielded the most anterior activity, tools the most posterior activity, and for animals, the activity was in between.
DEMENTIA MAY ERASE FROM THE DICTIONARY.
More recent research links deterioration of the anterior temporal lobe to the difficulties understanding what a word means exhibited by people with some types of dementia. Although people with Alzheimer's disease most commonly show this abnormality, it is most prominent in a type of aphasia [loss of ability to understand or express speech] known as semantic dementia. When you speak with these individuals, they may start off sounding normal, but you will notice that they refer to all sorts of different items as the ‘thing’ or a similar word. As you talk with them further, you will discover that they do not know what specific terms mean, such as ‘medicine’ or ‘shoe’ — two examples from one of my patients. Someone may forget the word hippopotamus when shown a picture and lose all the knowledge they once had about this (e.g., it is an African animal that lives in rivers). However, unlike Alzheimer's disease, memory for day-to-day events may be adequate. People may also have difficulty recognizing what things are. At later stages, personality is often affected.
SEMANTIC MEMORY IN OTHER BRAIN REGIONS.
Just as our knowledge is not limited to words, neither is our semantic memory limited to the left temporal lobe. The right temporal lobe has been linked to knowledge of nonverbal information (such as a golf ball's weight versus a ping-pong ball) and facial recognition. Other parts of the brain also participate in semantic memory. For example, Frank Sinatra singing ‘Fly Me to the Moon’ sounds like it is stored in your auditory association cortex in your superior temporal lobe. Your image of a brilliant white Tesla is stored in your visual association cortex in your occipital lobes. And the feeling of tulip petals resting on your cheek is stored in your sensory association cortex in your parietal lobe.
SEMANTIC MEMORY DOES NOT DECLINE IN AGING.
Can improving your semantic memory help you do a crossword puzzle? Absolutely. Not only does semantic memory store the meaning of words and nonverbal concepts, but it also stores the relationships within and between terms and concepts.
For example, your semantic memory of the band Pink Floyd may be linked to the President of the United States in the following way: Pink Floyd's album Dark Side of the Moon may be connected in your semantic memory to moon landings, which is then connected to astronauts, to John Glenn, to senators, to politicians, and to presidents.
BOTTOMLINE
Semantic memory does not decline in normal aging. As you continue to learn new information throughout your life, your vocabulary and ability to solve crossword puzzles may improve with age. Scheduling regular periods of rest without distraction could help us all hold onto new material a little more firmly. In the age of information overload, it's worth remembering that our smartphones aren't the only thing that needs a regular recharge. Our minds do too.
References
https://pubmed.ncbi.nlm.nih.gov/27383595/
https://www.sciencedirect.com/science/article/abs/pii/S0010945219300218
Published 11/2/2020
Dr. Amar Singh, MD, and Dr. Poonam Singh, MD, are board-certified by the American Board of Internal Medicine and American Board of Obesity Medicine. They specialize in preventing, treating, and reversing chronic diseases using an evidence-based holistic approach. They are specifically interested in weight management, hormone re-balancing, and longevity. The American College of Physicians has recognized them as Fellows, FACP, for their excellence and contributions made to both medicine and the broader community. They enjoy teaching, volunteering, and advocating for their patients. Their mission is to share simple, effective, and proven strategies that lead to meaningful, sustainable, and long-lasting well-being.
Long Haulers: a tragedy
Suppose you are suddenly stricken with COVID-19. You have become very ill for several weeks. On awakening every morning, you wonder if this day might be your last. And then you begin to turn the corner. Every day your worst symptoms - the fever, the terrible cough, the breathlessness - get a little better. You are winning, beating a life-threatening disease, and you no longer wonder if each day might be your last. In another week or two, you’ll be your old self.
But weeks pass, and while the worst symptoms are gone, you’re not your old self — not even close. You can’t meet your responsibilities at home or work: no energy. Even routine physical exertion, like blowing leaves, you feeling exhausted. You ache all over. You’re having trouble concentrating on anything, even watching TV; you’re unusually forgetful; you stumble over simple calculations. Your brain feels like it’s in a fog. Your doctor congratulates you: the tests can no longer detect the virus in your body. That means you should be feeling fine. But you’re not feeling okay. You look better on paper than you feel. You try to wonder if this is depression or even PTSD. You seek the treatment and are disappointed.
What?
Tens of thousands of people in the United States have such a lingering illness following COVID-19. In the US, we call them post-COVID “long haulers.” Britishers call it “long COVID.” Although there is no formal definition of the term post-COVID long haulers, it is reasonable to include anyone diagnosed with COVID-19, or very likely to have been infected by it, who has not returned to their pre-COVID-19 level of health and function after six months.
The list of symptoms is long and variable. The most common include:
Coughing: one of the most common symptoms
Ongoing, sometimes debilitating, fatigue
Body aches
Joint pain
Shortness of breath
Chest pain
Change in heart rate
Chills
Night sweats
Gastrointestinal issues
Loss of taste and smell — even if this did not occur during the height of their illness
Difficulty sleeping
Headaches
Brain fog: unusually forgetful, confused or unable to concentrate even enough to watch TV. It can happen to anyone, regardless of initial severity of illness
Exhaustion: may be a form of what is called chronic fatigue syndrome, or myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Unfortunately for long-haulers, ME/CFS is not well understood, either.
There are patients who can go for a run and test completely normal. But they still don’t feel right. They aren’t back to their old selves, but we can’t fully define what’s wrong
Who?
How many people may become long haulers? We can only guess. Published studies and surveys conducted by patient groups indicate that 50% to 80% of patients continue to have bothersome symptoms three months after the onset of COVID-19 — even after tests no longer detect the virus in their body. In a recent article and a study from a team of British scientists, the Journal of the American Medical Association estimates about 10% of COVID-19 patients become long haulers. But it’s hard to quantify because it’s hard to define the length of time that lingering symptoms fit the long-haul COVID category.
Currently, we can’t accurately predict who will become a long hauler. Long-term COVID-19 appears to affect every kind of patient — from people who were hospitalized with severe COVID-19 to those with very mild bouts who recovered at home. It appears in regions with both high rates and low rates of COVID-19 infections. It attacks people who were battling other conditions before contracting COVID-19 and people who were completely healthy. And it afflicts both the old and the young. What’s new is that this affects some quite young people who were very healthy and never had other illnesses. As a recent article in Science notes, people only mildly affected by COVID-19 still have lingering symptoms, and people who were severely ill can be back to normal two months later. However, persistent symptoms are more likely to occur in people over age 50, people with two or three chronic illnesses, and people who became very ill with COVID-19.
Long haulers include two groups of people affected by the virus:
Those who experience permanent damage to their lungs, heart, kidneys, or brain may affect their ability to function.
Those who continue to experience debilitating symptoms despite no detectable damage to these organs. It has been speculated that many in this group will develop a condition called myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). ME/CFS can be triggered by other infectious illnesses — such as mononucleosis, Lyme disease, and severe acute respiratory syndrome (SARS), another coronavirus disease. The National Academy of Medicine estimates one million to two million people in the US with ME/CFS.
Why?
It’s so new that science is only beginning to grasp the phenomenon of long haulers. The vast majority of long haulers test negative for COVID-19 and there is no specific test to give them for lasting symptoms of the coronavirus. Unfortunately, we don’t know enough about the virus to test for its lingering effects. There are questions about why their fatigue goes on and on, and science just hasn’t solved them yet. We’re all learning in real-time.
Research is underway to test several theories. The most common theories about long-term COVID-19 patients:
the virus remains in their bodies in some small form. This doesn’t mean the virus is growing or that we can test for it, but this might mean their bodies are reacting to it or it’s still triggering ongoing inflammation
immune systems continue to overreact even though the infection has passed
Bottomline
For now, doctors affirm long haulers that it is real and encourage them to rest, recover, and be patient. We’re learning a lot at a very rapid pace, but we’re also a culture of wanting to know everything right now. The scientific process to figure out what’s going on … takes time. For pandemics, like the illnesses they generate, linger not only in our bodies but also in our minds, culture, and communities. What we choose to make of this lingering, and how we interpret the pandemic's sequelae, will be the true measure of our care.
References:
Published 11/1/2020
Dr. Amar Singh, MD, and Dr. Poonam Singh, MD, are board-certified by the American Board of Internal Medicine and American Board of Obesity Medicine. They specialize in preventing, treating, and reversing chronic diseases using an evidence-based holistic approach. They are specifically interested in weight management, hormone re-balancing, and longevity. The American College of Physicians has recognized them as Fellows, FACP, for their excellence and contributions made to both medicine and the broader community. They enjoy teaching, volunteering, and advocating for their patients. Their mission is to share simple, effective, and proven strategies that lead to meaningful, sustainable, and long-lasting well-being.
Is Laughter The Best Medicine?
Is it just an adage, or does it have any merit? Well, there is plenty of evidence to support it.
But hold on, why do we even have to talk about laughter? Isn’t it a natural thing? When did we unlearn laughing and trade in our happy faces for serious scowls? Close your eyes and drift back to visions of your childhood – long hours of playing with friends, riding bikes around the neighborhood till dark, and indulging at will in the joy of endless laughter. Slowly and without notice, your youthful silliness gave way to stodgy adult silence. You grew up, and with it came grown-up responsibilities. Moments of folly and jolly became far, and few between as the responsibilities of adult life got in the way.
Science of Silly
Do you know that reclaiming your joie de rire not only lifts your spirits but may also help you get healthier?
Happy heart
Laughter exerts a positive influence on the cardiovascular system. Strong emotions are known to stimulate the sympathetic nervous system, which increases both heart rate and blood pressure. In a study that exposed three groups of men to a humorous, sad, or neutral movie, only the sad movie caused a rise in blood pressure. In contrast, the blood pressure in participants watching the funny film remained stable. The authors concluded that a humorous stimulus might help buffer the rise in blood pressure. Pretty good side effect of having a bit of fun, especially if you’ve had, or are at risk for a heart attack!
Immune booster
Researchers at Loma Linda University in California exposed 52 men to a humorous video for one hour. Blood samples were taken before, during, and after revealed increases in protective natural killer cell activity and immunoglobulins, with some of these beneficial effects lasting as long as 12 hours after the intervention. The authors concluded that laughter might have significant benefits for the immune system.
Mental well-being
WHO estimate indicates that over 350 million people are estimated to suffer from depression, equivalent to 4.4% of the world's population. Major depression is one of the most common mental disorders in the United States, afflicting at least 7.1% of all U.S. adults. There is incontrovertible evidence that humorous stimuli and a healthy sense of humor are associated with lower levels of depression, loneliness, stress, and higher levels of self-esteem and quality of life. In a study, 60 older women with depression were randomly assigned to a laughter yoga group, an exercise group, or a control group. Similar improvements in mood were observed in the laughter yoga and exercise groups compared to the control group. Moreover, the laughter yoga group scored better than the other groups on the Life Satisfaction Scale.
In another study of 48 older patients with depression and 61 age-matched controls, participants exposed to four weekly laughter groups scored significantly lower on the Geriatric Depression Scale and had a better Pittsburgh Sleep Quality Index score than those in the control group.
In a 2010 review, Fonzi and colleagues summarised the effects of laughter on depression, finding that:
laughter improves mood directly and moderates the negative consequences of stressful events on mental well-being.
laughter stimulates regions of the brain involved in the development of depression and normalizes dysfunction of the hypothalamic-pituitary-adrenocortical system.
laughter has positive effects on social relationships and physical health, which can help depressed people to face the disease.
Helps Diabetes
For people with diabetes, healthy eating, regular activity, medication, and education are the cornerstones of management. But a healthy dose of laughter may be just what the doctor ordered. Japanese researchers studied the effects of laughter on after-meal blood glucose levels. Participants with type 2 diabetes ate a 500 calorie meal followed by an intentionally boring 40-minute lecture, with blood glucose levels measured two hours later. This was repeated on a different day but instead with a comedy show of the same duration. After the boring intervention, blood glucose levels rose 6.8 mmol/L, whereas blood glucose levels only rose to 4.3 mmol/L after the laughter treatment. A side dish of sweet laughter may prevent the post-meal increase in blood glucose levels.
Protects Kidneys in Diabetes
In a separate report based on the same study, the comedy show attendees also experienced desirable reductions in prorenin – an early warning sign for diabetic kidney disease. In a related study, the same researchers observed improvements in the renin-angiotensinogen system (linked to blood pressure and diabetes) and blood prorenin levels of participants with type 2 diabetes receiving six months of laughter therapy. Laughter treatments can stave off diabetic kidney disease. How cool is that?
Laugh without reason?
What about laughing for no good reason whatsoever? Is it possible to fake it until you make it and still reap the health benefits? Surprisingly both genuine and fake laughter produces the same happy chemistry. And this is the premise of laughter yoga. Laughter Yoga is a relaxed social experience where you get together in a group and do interactive chants and hand-clapping, act out silly hypothetical scenarios, imitate animals such as waddling penguins, or blow up your cheeks like a pufferfish – the possibilities are limitless! The childlike playfulness and simulated laughter which accompanies the exercises soon give way to genuine, contagious laughter. First started by Dr. Madan Kataria in 1995 as five people laughing for no reason in a park in India has since turned into a global phenomenon. There are now about 8000 laughter yoga clubs in 100 countries. It’s about being entirely in the moment, not thinking about your problems or things you have to do, or even how silly you feel, but allowing yourself and your mind time to play, release your inner child and give you some much-needed exercise.
Laughter is a wine for the soul. Like anything we do in life, laughter is a habit – the more you practice, the easier it becomes, and the more relaxed you feel. In a world that takes itself far too seriously, that’s certainly something we could all use. You don't stop laughing because you grow old. You grow old because you stop laughing!
References:
https://pubmed.ncbi.nlm.nih.gov/21241447/
https://pubmed.ncbi.nlm.nih.gov/20848578/
https://pubmed.ncbi.nlm.nih.gov/17540229/
https://pubmed.ncbi.nlm.nih.gov/19450597/
Published 8/23/2020
Dr. Amar Singh, MD, and Dr. Poonam Singh, MD, are board-certified by the American Board of Internal Medicine and American Board of Obesity Medicine. They specialize in preventing, treating, and reversing chronic diseases using an evidence-based holistic approach. They are specifically interested in weight management, hormone re-balancing, and longevity. The American College of Physicians has recognized them as Fellows, FACP, for their excellence and contributions made to both medicine and the broader community. They enjoy teaching, volunteering, and advocating for their patients. Their mission is to share simple, effective, and proven strategies that lead to meaningful, sustainable, and long-lasting well-being.
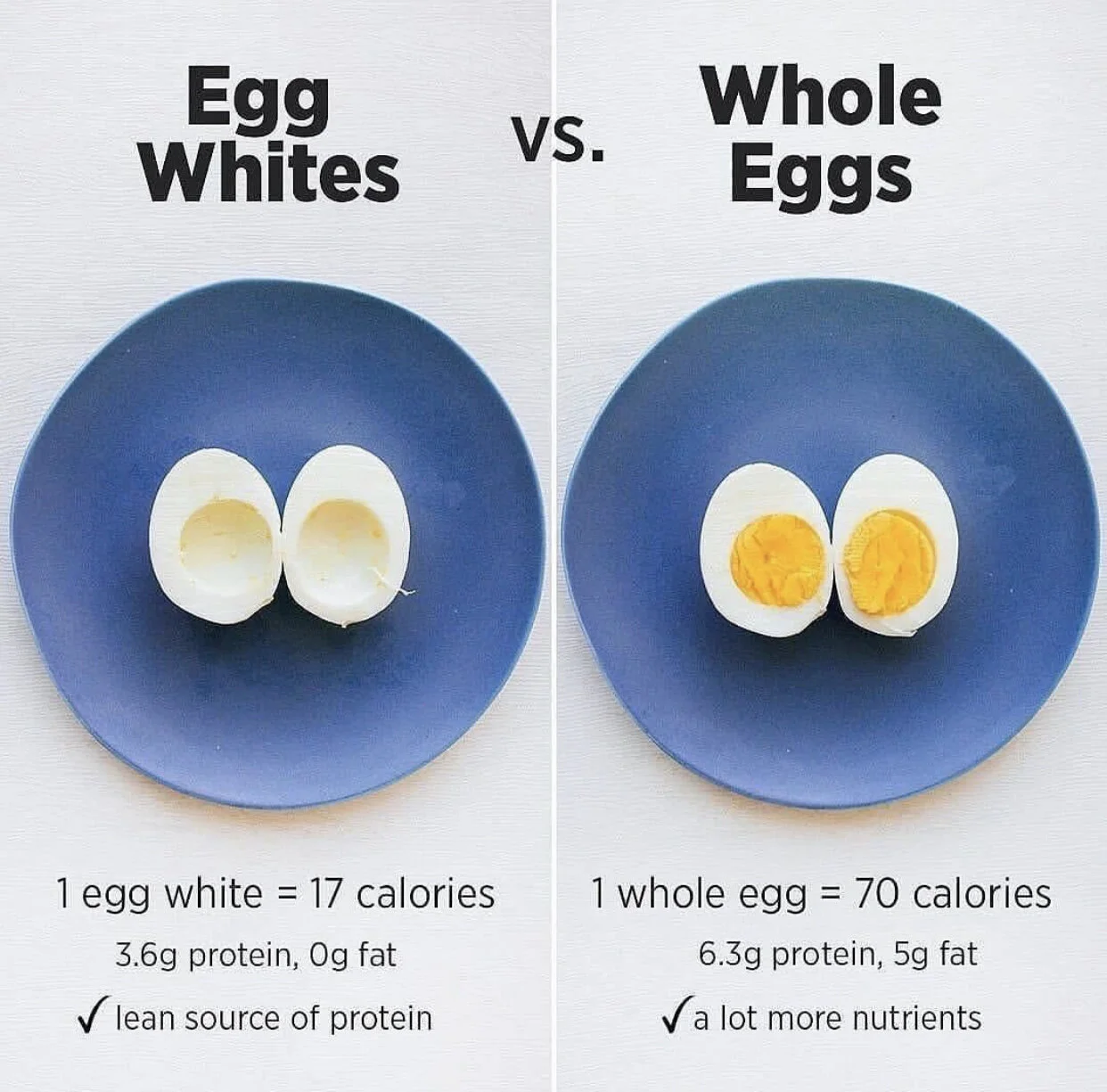
Stop Counting Eggs!
Go ahead and crack that egg. Yes, you can have it. But there are caveats. Read on.
Eggs are an essential whole food frequently consumed by people across populations and cultures, which affordably support societies’ nutritional needs.
So what does an egg have in it?
One large egg (50 grams):
72 calories
5 grams of fat (30% saturated, 50% monounsaturated fat and 16% is polyunsaturated fat)
70 milligrams of sodium
6 grams of protein.
The yolk contains all the fat and cholesterol, most of the calories, nearly half of the protein, zinc, B vitamins (including riboflavin and folate), vitamin A, iron, carotenoids (lutein and zeaxanthin), choline, and other nutrients.
White egg or the brown egg?
“Designer” eggs contain more lutein, vitamin E, and omega-3 fats. They come from chickens fed special diets. But they rarely provide enough extra nutrients to be worth their higher cost. Eggs that claim to be rich in omega-3s, for example, contain only a small amount compared to fatty fish, such as salmon.
Brown eggs are not more nutritious than white. Different breeds lay eggs with different shell colors. For example, Orpington hens lay brown eggs, and Leghorns lay white ones. Some breeds even lay blue or green eggs.
Yolk color depends on what the chicken ate: wheat and barley produce a light yolk, corn a medium-yellow yolk, and marigold petals a deep yellow. Though not a sure indication, darker yolks may have more omega-3s and carotenoids.
Organic eggs come from the chickens fed an organic diet, not that they are necessarily more nutritious.
Little history
Eggs have long been singled out as food for restriction in human nutrition, although they are widely available, affordable, nutrient-dense, and a rich source of high-quality protein. In the past, dietary guidelines recommended an upper limit of egg intake (2 or 3 eggs/wk or less) to prevent CVD since eggs are a significant dietary cholesterol source. This recommendation to limit egg consumption was based on the observation that dietary cholesterol increases blood cholesterol and that blood cholesterol increases with CVD. In the 2015–2020 edition of the Dietary Guidelines for Americans, an earlier recommendation to limit dietary cholesterol consumption to 300 mg/d was withdrawn due to the lack of adequate evidence. Epidemiologic studies on egg consumption and the risk of CVD are sparse. Research in recent years has mostly exonerated eggs since it turns out that saturated fat in food, rather than dietary cholesterol, has a more significant effect on blood cholesterol and the related risk of heart attack and stroke.
Good or Bad?
The association between egg consumption and cardiovascular disease risk has been a topic of intense debate during the past decade. In the past year, three published studies have reported conflicting findings. Recent studies have reignited the discussion on this controversial topic.
Two extensive, recent observational studies add to the evidence that most people can safely enjoy eating eggs without fear of endangering their heart health. The egg industry did not fund these studies.
A study published in the American Journal of Clinical Nutrition analyzed data from about 177,000 people in 50 countries. It found that moderate consumption of eggs (up to an egg a day) was not associated with a higher risk of CVD, early death, or elevated blood cholesterol levels, even in people with a history of CVD or diabetes. This new study updates a 1999 one that likewise found no connection between eggs and heart disease risk.
A study published in the British Medical Journal in March 2020 looked at data from more than 215,000 health professionals for three decades, after adjusting for age, lifestyle, and dietary factors. The researchers found that moderate egg consumption (one egg daily) is not associated with cardiovascular disease—including CVD and stroke. This should help reassure uneasy egg eaters. Interestingly, the researchers also found some evidence suggesting that eating one egg daily may be associated with lower heart disease risk in Asian populations. It’s plausible that finding may be affected by the overall dietary habits of Asians.
Bottomline
You can have one egg daily without increasing the risk of cardiovascular disease, stroke, or early death. However, high‐risk individuals, such as those with high cholesterol and those already with high dietary cholesterol intake levels, should be careful. And yes, eating bacon and sausage with your daily egg will undoubtedly increase your risk. While not essential, moderate egg consumption can be part of a healthy diet. Stop counting eggs and move to healthier overall dietary patterns.
References:
Published 8/21/2020
Dr. Amar Singh, MD, and Dr. Poonam Singh, MD, are board-certified by the American Board of Internal Medicine and American Board of Obesity Medicine. They specialize in preventing, treating, and reversing chronic diseases using an evidence-based holistic approach. They are specifically interested in weight management, hormone re-balancing, and longevity. The American College of Physicians has recognized them as Fellows, FACP, for their excellence and contributions made to both medicine and the broader community. They enjoy teaching, volunteering, and advocating for their patients. Their mission is to share simple, effective, and proven strategies that lead to meaningful, sustainable, and long-lasting well-being.
Are You Overeating Salt?
On average, Americans overeat salt — more than a teaspoon and a half a day. Most often, it doesn't come out of a shaker. It is hidden in the foods you eat. But is it terrible for your heart to overeat, or is that just a concern for people with certain risk factors?
What’s the difference between salt and sodium?
Sodium is a component of table salt (sodium chloride). One teaspoon of salt, 40 percent sodium, and 60 percent chlorine, has about 2,300 milligrams of sodium, the upper recommended limit. If you restrict sodium to 1,500 milligrams a day, that’s only two-thirds of a teaspoon of salt. Sodium is also a significant component of other food ingredients (preservatives) such as MSG (monosodium glutamate), baking soda (sodium bicarbonate), disodium phosphate, sodium benzoate, sodium propionate, sodium sulfite, and sodium nitrite/nitrate.
Salt is essential for life. The sodium in salt helps transmit nerve impulses and contract muscle fibers. It also works with potassium to balance fluid levels in the body. But you need only a tiny amount of salt to do this — less than one-tenth of a teaspoon per day. The average American gets nearly 20 times that much.
Is salt pretty bad for your heart?
In general, most researches link lower sodium intake with lower blood pressure and a lower risk of cardiovascular disease. Sodium has a definite effect on blood pressure. The result is more robust in people with high blood pressure (hypertension), a sustained blood pressure reading of 120/80 or higher.
How does salt elevate blood pressure?
When you overeat salt, your body holds onto the water to dilute it. This extra water increases your blood volume, which means your heart works harder because it's pushing more liquid through your blood vessels. More strenuous pumping by the heart puts more force on the blood vessels. Over time, this increased force can raise blood pressure and damage blood vessels, making them stiffer, which increases the risk of stroke, heart attack, and heart failure.
Do people respond differently to salt?
Research has found that certain people appear genetically more salt (sodium) -sensitive than others. These salt-sensitive people typically see more significant drops in their blood pressure when they eat less salt. Other people may not see the same benefit. However, most people benefit from being aware of salt in their diet and limit their use.
Who is salt-sensitive?
About 60% of individuals with high blood pressure are salt-sensitive. In comparison, only 25% of people with normal blood pressure; however, they may develop high blood pressure later, since salt sensitivity increases with age and weight gain. These estimates come from studies of people who underwent formal testing for salt sensitivity. This arduous and costly process involves carefully increasing the sodium in the diet while monitoring blood pressure and continuously measuring how much sodium leaves the body in the urine. New research shows that salt intake raises blood pressure because it makes it harder for the cardiovascular system to juggle blood pressure regulation and body temperature simultaneously. The American Heart Association considers salt sensitivity to be nearly as strong a cardiovascular risk factor as chronic high blood pressure. Lowering high blood pressure reduces the risk of heart disease and stroke.
About 33% of people with high blood pressure appear to be salt-resistant. Their blood pressure doesn’t respond as vigorously to a reduction in sodium intake. Currently, it is not practical for providers to try to determine whether a patient is salt-sensitive or not.
Salt sensitivity survival advantage?
Millions of years ago, when our distant ancestors roamed around Africa, salt was scarce in their diets. The human body depends on sodium to maintain average blood volume, transmit nerve impulses, contract muscle fibers, and other vital functions. An ability to hold on to this nutrient was a survival advantage. And as humans evolved, infections causing sodium loss by diarrhea and vomiting were among the most severe threats to surviving into adulthood. This well founded theory may explain why humans have gene variants (Thrifty gene) that make them sensitive to salt.
Thrifty gene hypothesis explains why certain groups of people are more predisposed to a variety of diseases. Thrifty genes enable individuals to collect and process food efficiently, hold on to calories and sodium, and provide for periods of food shortage (feast and famine). The modern-day environment is full of salty, high-calorie foods. So these variants potentially contribute to high blood pressure and obesity — two leading contributors to heart disease. Why haven't these variants been "washed out" of the gene pool, since they no longer help us survive in this modern world? The diseases caused by these thrifty genes usually kill people in adulthood after they have procreated. So these gene variants persist in the human gene pool.
How much salt is too much?
If you don’t have any health issues: take 2,300 milligrams (mg) per day or less. It is approximately one teaspoon of salt.
If you have high blood pressure or cardiovascular disease: take 1,500 mg or less of sodium each day. It is ⅔ teaspoon of salt.
An average person consumes about 3,600 mg a day. So, this would mean cutting out about a third of the salt for most people.
Why do processed foods contain so much salt?
Traditionally, salt has been used to preserve food. These days salt is used to enhance flavor. Paradoxically, salt can make foods taste sweeter by blocking the bitterness of individual ingredients. It’s possible to reduce sodium without adversely affecting quality and taste. Many food companies have been lowering the salt co’ salt content due to increasing pressure in recent years.
Will cutting salt make food unappetizing?
You won’t miss the salt for long. Though we have an innate liking for salt, individual preferences are learned mainly and can be unlearned. It takes several weeks for your taste buds to adapt to a lower sodium level, but what once tasted just right will eventually feel too salty—and you will begin to notice flavors that were previously masked by the salt. A low-sodium diet tastes best when filled with fresh foods, like fruits and vegetables, that are naturally low in sodium but rich in flavor and reduced-sodium processed foods.
Does rinsing canned foods lower the sodium?
Yes, some. A half-cup of canned beans has about 350 to 500 milligrams of sodium. You can reduce this by about one-third if you drain and rinse the beans first. That still leaves most of the sodium, however. Alternatively, look for low-salt/sodium (and wash those too) or no-salt-added versions. Or prepare dry beans, which have negligible sodium, by soaking and cooking them. You can also rinse canned tuna and canned vegetables.
How can you reduce sodium in your diet?
Crackers, snacks, and canned food typically contain a lot of sodium. Avoid the ‘low fat’ or ‘low calorie’ version of food as it may contain a lot more sodium than the ‘regular’ version.
Try to ensure that each serving of food has less than 100 mg of sodium.
Substitute the salt for spices and other flavor enhancers.
Black pepper, cinnamon, turmeric, fresh basil, chili peppers, lemon juice, herbs, garlic, ginger, citrus, vinegar, and wine. They will excite your palate with a lot less sodium.
Use healthy fats to flavor food.
Roasted nuts and avocados to olive, canola, soybean, oils — can add a rich flavor to foods, minus the salt.
Roast, steam, sear and sauté, and roast.
Roasting brings out the natural sweetness of many vegetables and the taste of fish and chicken. If you steam some dishes, perk them up with a finishing drizzle of flavorful oil and a squeeze of citrus. Searing or sautéing foods in a pan build flavor.
Get your whole grains from sources other than bread.
Even whole-grain bread, though a healthier choice than white, can contain much sodium. Bread contains quite a bit of salt — not just for flavor but also for ensuring that the dough rises properly. You can skip that extra salt when you look for whole grains outside of baking. For example, instead of toast with breakfast, cook up steel-cut oats, farro, or other intact whole grains with fresh or dried fruit.
Shop for raw ingredients with maximum natural flavor, thereby avoiding the need to add as much (if any) sodium. Shop for peak-of-season produce from farmers' markets and your local supermarket.
Most of the salt that Americans consume comes from prepared and processed foods. Making your meals, rather than purchasing premade items, can give you more control over how much salt is in your diet. Opt to season food with herbs or spices instead of salt.
References:
https://www.cdc.gov/heartdisease/sodium.htm
Published 8/15/20
Dr. Amar Singh, MD, and Dr. Poonam Singh, MD, are board-certified by the American Board of Internal Medicine and American Board of Obesity Medicine. They specialize in preventing, treating, and reversing chronic diseases using an evidence-based holistic approach. They are specifically interested in weight management, hormone re-balancing, and longevity. The American College of Physicians has recognized them as Fellows, FACP, for their excellence and contributions made to both medicine and the broader community. They enjoy teaching, volunteering, and advocating for their patients. Their mission is to share simple, effective, and proven strategies that lead to meaningful, sustainable, and long-lasting well-being.
Do You Have Restless Legs?
You may know the feeling. You’re relaxing on the couch, watching some Netflix, and suddenly you get the overwhelming urge to move your legs. You may even feel some pain or a prickling sensation. Moving your legs around helps some, but once you stop, the urge starts up again. Or perhaps you experience it while you’re lying in bed, making it difficult to sleep. The phenomenon is known as restless legs syndrome (RLS), and it affects one in ten Americans. Restless legs syndrome, also called Willis-Ekbom disease, is a sleep disorder that causes an intense, often irresistible urge to move your legs, arms, or other parts of the body. Most people reach out to their healthcare providers for sleep difficulties.
Symptoms of RLS :
Leg or arm discomfort: uncomfortable limb sensations - creeping, itching, pulling, crawling, tugging, throbbing, burning, or gnawing. The "creepy-crawlies."Most common at bedtime but can happen during the day at other times of limb inactivity (like a long car or plane ride, sitting for a long time).
Urge to move legs or arms: an uncontrollable urge to move limbs, especially when sitting or lying down. Movements occur every 20 to 40 seconds for a few minutes or a few hours at a time.
Sleep disruption: The leg sensations caused by RLS make it harder to fall asleep or return to sleep after awakening by the leg sensations. Many times people get out of bed and try to walk it off, unsuccessfully. Sleeping partners can also suffer, as most people with RLS also experience involuntary muscle movements called periodic leg movements of sleep (PLMS). These typically occur in the foot, ankle, or knee every 15 to 30 seconds, lasting for about two seconds and sometimes longer. People without RLS can also experience PLMS.
Bedtime behavior problems: overwhelming urge to get out of bed
Daytime sleepiness: sleep deprivation usually leads to daytime tiredness.
Behavior and work performance problems: nighttime sleep disruption may cause daytime irritability, moodiness, difficulty concentrating, hyperactivity, and compromised work performance.
Why does RLS happen?
Inherited: Up to 92% of patients with RLS have a first-degree relative with the disorder. These patients tend to develop symptoms earlier in life (before age 45) than those with RLS without the genetic link.
Medical problems are closely associated with the development of RLS, including:
Iron deficiency.
Underactive thyroid.
Depression.
Fibromyalgia.
Parkinson's disease.
Kidney disease.
Diabetes.
Rheumatoid arthritis.
Nerve disorders.
Sleep Apnea.
Pregnancy. (especially in the last trimester; in most cases, symptoms usually disappear within 4 weeks after delivery)
Dialysis.
Medications: certain medications that may aggravate RLS symptoms, such as anti-nausea drugs (e.g., prochlorperazine or metoclopramide), antipsychotic drugs (e.g., haloperidol or phenothiazine derivatives), antidepressants that increase serotonin (e.g., fluoxetine or sertraline), and some cold and allergy medications that contain older antihistamines (e.g., diphenhydramine)
Caffeine, nicotine, and alcohol can also make symptoms worse.
How to get rid of RLS?
During the day, drink adequate fluids. Drink a little extra when working or playing in hot weather or take medications that cause you to excrete excess water, such as diuretics. Build-in frequent walking and stretching the time between periods of sitting or resting. Wearing supportive shoes with firm arch support and laces or secure fastenings.
Before going to bed, massage your leg muscles, gently stretch your legs or slowly pedal a stationary bike for a few minutes, or take a short walk, take a warm bath, or apply heating pads.
Avoid caffeine, nicotine, and alcohol, especially within several hours of bedtime.
Daily exercises may help to decrease RLS symptoms.
Schedule activities that require prolonged sitting or reclining—like car and plane travel and medical appointments—in the morning rather than the afternoon.
Dietary iron may sometimes be enough to treat RLS. Iron is an essential mineral that we get from our diets, such as red meat, cooked soybeans, cooked lentils, ground turkey, and fortified bread and breakfast cereals. We need only a small amount of dietary iron each day: 8 milligrams per day for adult men and women after menopause.
Oral iron supplements may be used when iron stores are deficient. The usual starting dose is one tablet of 325 milligrams of ferrous sulfate once per day. It's best absorbed when your stomach is acidic, so take it on an empty stomach or take it with vitamin C to acidify the stomach. Oral iron can cause stomach upset and constipation, so it may help take it every other day rather than daily. In some cases, an iron infusion may be needed.
Magnesium deficiency may make RLS worse. If magnesium level is on the lower side, magnesium supplementation may be helpful.
Medication may also be used when there is no iron deficiency and symptoms are troubling. There are now five FDA-approved medications for people with severe and frequent symptoms of RLS.
What is the prognosis?
RLS is generally a lifelong condition for which there is no cure. However, current therapies can control the disorder, minimize symptoms, and increase periods of restful sleep. Symptoms may gradually worsen with age, although the decline may be somewhat faster for individuals who also suffer from an associated medical condition. RLS diagnosis does not indicate the onset of another neurological disease, such as Parkinson’s disease. Besides, some individuals have remissions—periods in which symptoms decrease or disappear for days, weeks, months, or years—although symptoms often eventually reappear. If RLS symptoms are mild, do not produce significant daytime discomfort, or do not affect an individual’s ability to fall asleep, the condition does not have to be treated.
See your healthcare provider if your condition bothers you or if it keeps you from getting a good night's sleep.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6280211/
https://www.mp.pl/paim/en/node/4148/pdf
Published 8/13/20
Dr. Amar Singh, MD, and Dr. Poonam Singh, MD, are board-certified by the American Board of Internal Medicine and American Board of Obesity Medicine. They specialize in preventing, treating, and reversing chronic diseases using an evidence-based holistic approach. They are specifically interested in weight management, hormone re-balancing, and longevity. The American College of Physicians has recognized them as Fellows, FACP, for their excellence and contributions made to both medicine and the broader community. They enjoy teaching, volunteering, and advocating for their patients. Their mission is to share simple, effective, and proven strategies that lead to meaningful, sustainable, and long-lasting well-being.
-
July 2024
- Jul 2, 2024 Conquering Mount Kilimanjaro: A Journey Beyond the Summit Jul 2, 2024
-
March 2024
- Mar 28, 2024 Shingles Explained: What Triggers This Painful Rash and What to Do About It? Mar 28, 2024
- Mar 1, 2024 Should you believe every medical news headline? Mar 1, 2024
-
February 2024
- Feb 18, 2024 Can you boost your immune system? Feb 18, 2024
-
January 2024
- Jan 6, 2024 Live Longer Live Better with Strength Training Jan 6, 2024
-
May 2022
- May 25, 2022 Lemon Water May 25, 2022
-
December 2021
- Dec 4, 2021 Should You Take Turmeric? Dec 4, 2021
-
November 2021
- Nov 10, 2021 Weight Balance: Chemistry or Choices? Nov 10, 2021
-
August 2021
- Aug 13, 2021 Walking Through Grief Aug 13, 2021
-
March 2021
- Mar 3, 2021 Medical Weight Management Mar 3, 2021
-
February 2021
- Feb 23, 2021 It's Cold Outside! Do Your Joints Hurt? Feb 23, 2021
- Feb 3, 2021 How To Curb Sugar Craving Feb 3, 2021
-
January 2021
- Jan 25, 2021 How To Stop Unconscious Overeating? Jan 25, 2021
- Jan 17, 2021 Ouch! Why your body hurts? Jan 17, 2021
- Jan 10, 2021 Quick Guide: Decoding Blood Test Results Jan 10, 2021
- Jan 2, 2021 This will make you drink more Jan 2, 2021
-
December 2020
- Dec 26, 2020 Good Bye, 2020. Hello, 2021! Dec 26, 2020
- Dec 17, 2020 Why should you take the COVID19 vaccine? Dec 17, 2020
- Dec 11, 2020 Can you smell a rose? Dec 11, 2020
- Dec 9, 2020 Twelve things doctors wish patients knew about flu shots Dec 9, 2020
-
November 2020
- Nov 28, 2020 How To Protect Your Vision From A Silent Enemy Nov 28, 2020
- Nov 25, 2020 Getting Back To Gratitude Nov 25, 2020
- Nov 20, 2020 Oil for Brain Health? Nov 20, 2020
- Nov 14, 2020 Coronasomnia Nov 14, 2020
- Nov 6, 2020 Are crossword puzzles becoming difficult? Nov 6, 2020
- Nov 1, 2020 Long Haulers: a tragedy Nov 1, 2020
-
August 2020
- Aug 23, 2020 Is Laughter The Best Medicine? Aug 23, 2020
- Aug 21, 2020 Stop Counting Eggs! Aug 21, 2020
- Aug 15, 2020 Are You Overeating Salt? Aug 15, 2020
- Aug 13, 2020 Do You Have Restless Legs? Aug 13, 2020
- Aug 8, 2020 Key Benefits of the Anti-Inflammatory Diet Aug 8, 2020
- Aug 7, 2020 Tips To Prevent Pain While Working or Studying Aug 7, 2020
- Aug 4, 2020 DOSE of Happiness Aug 4, 2020
- Aug 2, 2020 How To Tame Emotional Eating Aug 2, 2020
-
July 2020
- Jul 27, 2020 How to maintain hormone balance Jul 27, 2020
- Jul 25, 2020 Fatty Liver Jul 25, 2020
- Jul 17, 2020 Coffee Ways Jul 17, 2020
- Jul 4, 2020 Top Twelve Reasons Why Water Matters Jul 4, 2020
-
June 2020
- Jun 28, 2020 How Fit Are You? Jun 28, 2020
- Jun 21, 2020 Father’s Day Jun 21, 2020
- Jun 20, 2020 Does Social Media Make You Lonely? Jun 20, 2020
- Jun 13, 2020 Can Diet Prevent Diabetes? Jun 13, 2020
- Jun 9, 2020 What to do to gain up to 10 extra years of disease-free life Jun 9, 2020
-
May 2020
- May 31, 2020 Regaining Calm During Crisis May 31, 2020
- May 31, 2020 Tips for Healthy Eating When Routines Drastically Change May 31, 2020
Sign up and you’ll never miss a post.